Anthrax: How do Anthrax disease Affect Animals in Livestock industry:
Learn More about Anthrax in Animals
Anthrax in Animals, covering all essential aspects:
Anthrax in Animals – Expanded Overview
1. Causative Agent
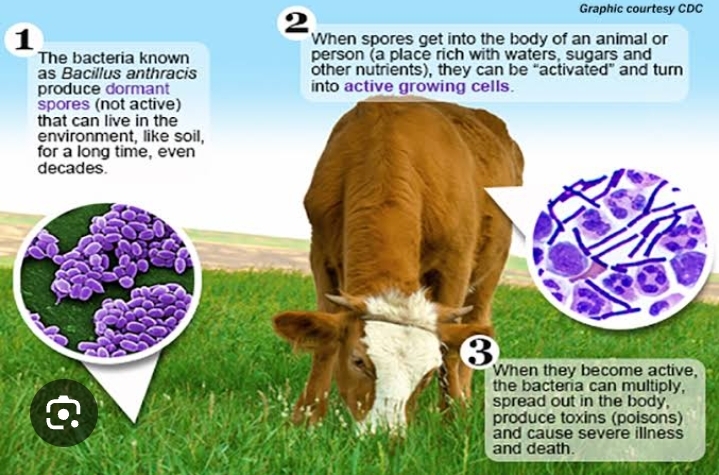
Anthrax is caused by Bacillus anthracis, a spore-forming, rod-shaped, Gram-positive bacterium. The spores are:
- Extremely resilient
- Capable of surviving in harsh environmental conditions for decades
- Found in soil, animal products, and contaminated water
The spores germinate into active bacteria when they enter a host, causing infection.
2. Anthrax Susceptible Species
The infection primarily affects herbivorous mammals, especially:
- Cattle
- Sheep
- Goats
- Horses
- Deer
Occasionally, pigs, carnivores, and humans (as a zoonotic disease) may become infected.
3. Modes of Anthrax Transmission
Animals contract this disease in several ways:
- Ingestion: Most common route — from contaminated pasture, feed, or water
- Inhalation: Less common; spores are inhaled from soil or dust
- Through skin wounds: Entry of spores via cuts or abrasions
- Insect bites: Mechanical transmission by biting flies (rare)
Outbreaks often occur after heavy rains or drought, which bring spores to the surface.
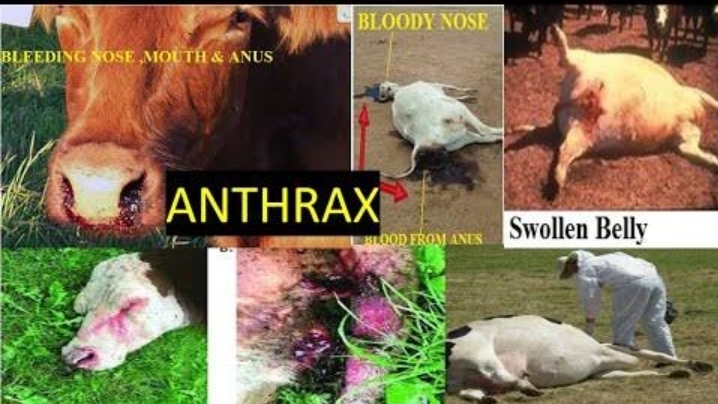
4. Clinical Signs and Symptoms
Symptoms vary based on the species and the form of infection:
Peracute (sudden death) – common in cattle and sheep:
- Sudden collapse and death
- Blood oozing from nose, mouth, anus
- No rigor mortis (body remains limp)
- Rapid bloating and decomposition
Acute/Subacute (more common in pigs and horses):
- High fever (up to 42°C / 107.6°F)
- Labored breathing
- Trembling, staggering
- Swelling of the throat, neck, or lower abdomen
- Bloody diarrhea or discharges
Chronic form (rare):
- Localized swelling
- Ulcerative lesions
- Progressive emaciation
5. Anthrax disease Pathogenesis
- Spores enter the body and germinate into active bacteria
- Bacteria multiply and produce toxins: Edema toxin, lethal toxin, and protective antigen
- These toxins cause severe tissue damage, hemorrhage, and shock
- Death often results from toxemia and septicemia

6. Diagnosis of an Anthrax disease
Ante-mortem (in live animals):
- Blood smear stained with polychrome methylene blue (shows blue-stained capsules)
- Culture of blood or tissues
- PCR (polymerase chain reaction) for DNA confirmation
Post Mortem:
- Not recommended due to spore formation risk
- If done, observe for:
- Black, tar-like, unclotted blood
- Enlarged, soft spleen
- Hemorrhagic lymph nodes
7. Treatment of Anthrax
- Must be administered early in the course of disease
- Antibiotics:
- Penicillin G
- Oxytetracycline
- Doxycycline
- Ciprofloxacin (rare in animals, used in humans)
- Supportive therapy (fluids, antipyretics) may help
How to prevent Anthrax:
8. Prevention and Control Measures of Anthrax disease
Vaccination:
- Annual vaccination in endemic regions with the Sterne strain live spore vaccine
- Do not vaccinate sick animals or animals under antibiotic treatment
Outbreak Control Measures:
- Immediate quarantine of affected area
- Do NOT open carcasses — opening exposes the blood to air and allows spores to form
- Safe disposal of carcasses:
- Burn completely or
- Deep burial (2 meters or more) with lime
:
Disinfection Process of Anthrax:
- Use 10% formalin or bleach on contaminated areas and equipment
Surveillance and Reporting:
- Report suspected cases to veterinary authorities
- Maintain records and conduct follow-up surveillance
9. Public Health Significance (Zoonosis)
Anthrax is a notifiable zoonotic disease:
- Humans can be infected through:
- Handling infected animals
- Contact with contaminated wool/hides
- Inhalation of spores (in industrial settings)
- Eating undercooked infected meat
Forms in humans:
- Cutaneous (most common, least deadly)
- Inhalation (rare, often fatal)
- Gastrointestinal
- Injectional (rare, among drug users)
Use protective clothing and hygiene protocols when handling animals or carcasses.
10.
Impact of Anthrax disease
- High mortality in livestock
- Loss of meat, milk, hides
- Trade restrictions and quarantines
- Costs of vaccination, disinfection, and surveillance
Check other: Animal Diseases
Also Read About: Available Vacancies
Introduction to Anthrax
Anthrax is a serious disease caused by the bacterium Bacillus anthracis, which primarily affects herbivorous animals. The disease is most prevalent in areas where environmental conditions allow disease spores to survive in the soil for long periods. These spores are highly durable and can remain dormant for years, becoming active when environmental conditions are favorable. Animals typically contract the disease through ingestion or inhalation of the spores while grazing.
Animals Most Affected
The animals most commonly affected by anthrax are domestic herbivores such as cattle, sheep, goats, and horses. These animals are especially vulnerable because they graze close to the ground where spores are often found. Wild herbivores, including bison, deer, various antelope species, and larger mammals like elephants and hippos, are also susceptible. In some cases, outbreaks in wild animal populations result in significant die-offs. For example, a 2016 anthrax outbreak in Siberia killed thousands of reindeer, while African national parks have witnessed similar devastating effects on hippo and elephant populations.
Anthrax to Carnivores and Scavengers
Carnivores and scavengers, such as lions, hyenas, and vultures, can be exposed to anthrax when they consume infected carcasses. However, they are generally more resistant to the disease compared to herbivores. Despite this, they can still spread the spores by scavenging, which helps disseminate the disease further. Human cases of anthrax are rare but can occur through direct contact with infected animals or their products, posing a risk particularly in agricultural, veterinary, or rural settings where people may consume contaminated meat.
Geographical Distribution
This disease is most common in regions with environmental conditions that support the survival of anthrax spores in the soil. In sub-Saharan Africa, countries like Namibia, Zambia, Zimbabwe, and Botswana are frequently affected by outbreaks, particularly among wildlife. In Asia, countries such as India and Bangladesh experience frequent livestock infections, largely due to inadequate veterinary services and insufficient vaccination programs. Central Asia, including Kazakhstan and Mongolia, has also seen large outbreaks, particularly among saiga antelope.
Most Regions Anthrax Affect the Most
In the United States, The outbreaks occur sporadically, especially in southern states like Texas, Louisiana, Mississippi, Oklahoma, and South Dakota, where dry conditions and alkaline soils promote the persistence of anthrax spores. Australia also faces occasional outbreaks, particularly in its northern and eastern regions. While Europe and the Middle East experience fewer outbreaks, countries like Turkey, Iran, and parts of Eastern Europe still report occasional cases.
Environmental Factors and the Spread
Environmental changes such as droughts, floods, or soil disturbances can expose anthrax spores by bringing them to the surface, increasing the likelihood of infection for grazing animals. Because anthrax spores can survive in the soil for many years, the disease remains a persistent threat to both livestock and wildlife populations. Effective management, including regular surveillance, vaccination, and rapid response to outbreaks, is crucial for controlling the disease and preventing its spread.
Conclusion
Anthrax remains a significant threat in many parts of the world, particularly in regions where the conditions support the survival of spores. While it primarily affects herbivores, carnivores and humans can also be exposed. With proper veterinary care, surveillance, and vaccination programs, the risk of disease outbreaks can be managed, reducing the impact on animal populations and preventing public health risks.