Find Out How Rabies Affect Animals in Our Veterinary Industry
Animal Disease Overview
**Rabies Disease Overview**:
—
### **Rabies Disease Overview**
#### **Causes:**
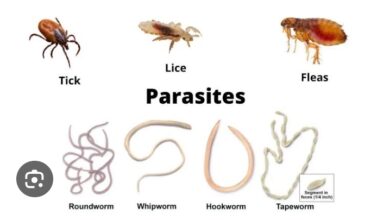
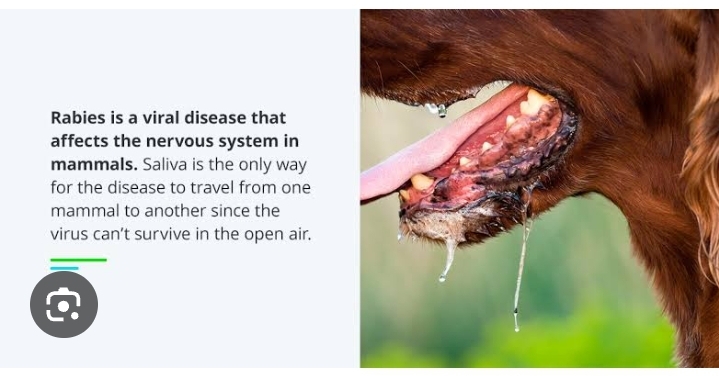
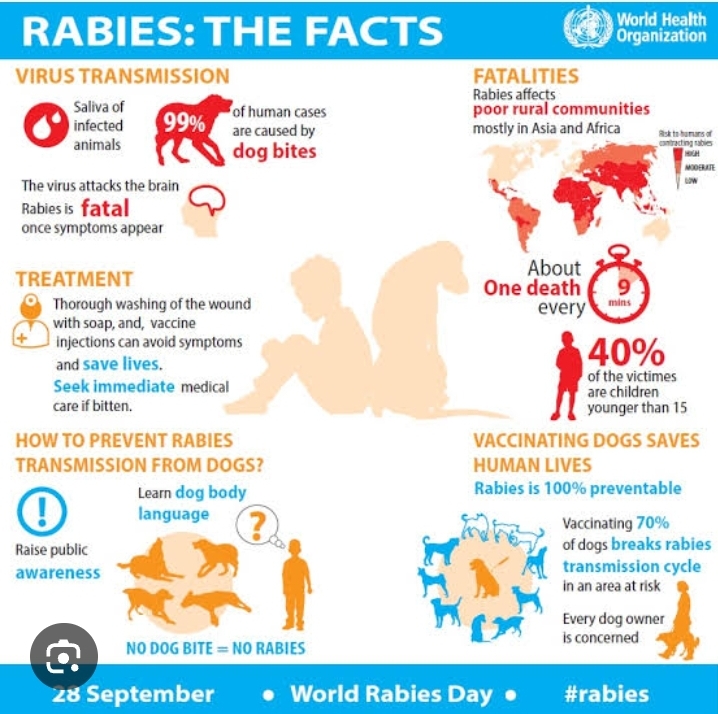
Rabies is caused by a **lyssavirus**, which infects the nervous system, specifically targeting the brain and spinal cord. The virus is primarily transmitted through the saliva of infected mammals. It most commonly spreads through **bites or scratches** from an infected animal, but can also be contracted through **mucous membranes** (such as the eyes, mouth, or nose) if the saliva of an infected animal comes in contact with them.
The animals most commonly associated with rabies transmission include:
– **Dogs** (especially in developing countries with poor vaccination practices)
– **Bats** (which are the most common source of rabies transmission to humans in certain areas, such as the U.S.)
– **Foxes**, **raccoons**, **skunks**, and **mangoose** (in certain regions)
– **Other wild animals**, including **coyotes** and **jackals**
Rabies is not transmitted through casual contact, such as touch, air, or sharing food. However, it is highly contagious among mammals when there is direct contact with the virus in saliva or through a bite.
#### **Impacts:**
Rabies has devastating effects on both the individual and the community, primarily due to its high fatality rate if untreated. The disease primarily impacts the **central nervous system (CNS)**, specifically the brain, causing severe inflammation and dysfunction in the neural pathways. The progression of the disease is rapid and can result in death within **days to weeks** once symptoms appear.
– **Neurological Damage:** Rabies causes inflammation in the **brain** (encephalitis), leading to the gradual breakdown of brain function.
– **Physical and Mental Effects:** Victims often experience significant **pain**, **paralysis**, **hallucinations**, **confusion**, and severe **agitation**.
– **Fatal Outcome:** If not treated in the early stages, rabies leads to a **coma**, **respiratory failure**, and eventual **death** from cardiac arrest or organ failure.
The disease is not only a public health threat but also a burden on the healthcare system due to the urgent need for intervention and treatment following exposure.
#### **Symptoms:**
Rabies symptoms typically appear **1 to 3 months** after exposure to the virus, but the incubation period can be shorter or longer depending on the severity and location of the bite. Symptoms can be broken down into stages:
**1. Early Stage:**
– **Fever**: An elevated body temperature due to infection.
– **Headache**: A general headache or discomfort is common.
– **Fatigue and Weakness**: The person feels tired and weak.
– **Tingling or Itching at the Bite Site**: The bite or scratch site may become painful and cause unusual sensations.
**2. Acute Stage (Neurological Phase):**
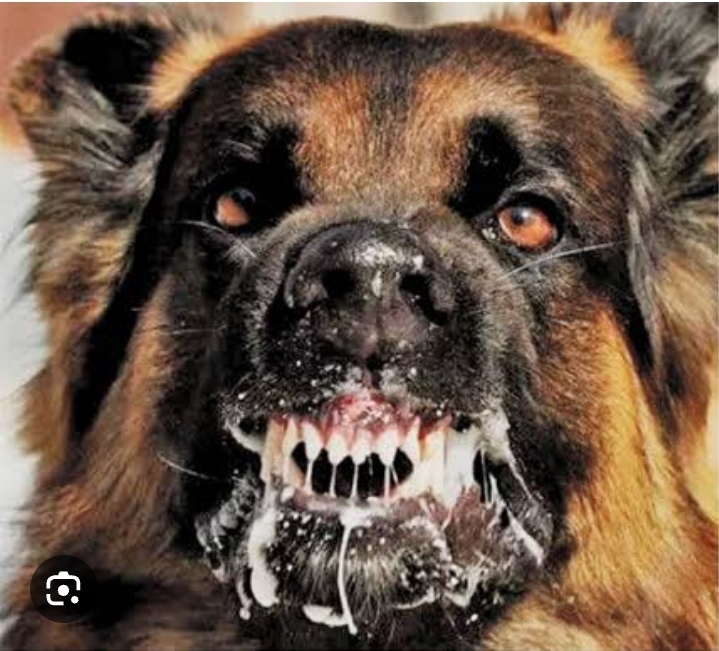
– **Painful Swallowing (Hydrophobia)**: Difficulty swallowing and a fear of water due to spasms in the throat.
– **Aerophobia**: Fear of drafts or air moving around the face, caused by spasms in the respiratory muscles.
– **Confusion and Agitation**: The individual may exhibit erratic behavior, confusion, and paranoia.
– **Hallucinations and Delirium**: The infected person may experience visual or auditory hallucinations.
– **Severe Muscle Spasms**: The virus causes muscle contractions and seizures, affecting motor control.
– **Paralysis**: Gradual paralysis starts in the limbs and spreads to the respiratory muscles, leading to difficulty breathing.
**3. Final Stage:**
– **Coma**: The person falls into a coma as the brain stops functioning properly.
– **Respiratory Failure**: Difficulty in breathing as the muscles responsible for respiration stop working, eventually leading to death.
Rabies progresses rapidly, and once these severe symptoms appear, the disease is almost always fatal.
#### **Treatments:**
Unfortunately, **no effective treatment** currently exists once the symptoms of rabies have appeared. The virus is almost universally fatal once the clinical signs are visible. However, **post-exposure prophylaxis (PEP)** is highly effective if administered promptly before the onset of symptoms. PEP involves a combination of treatments to prevent the virus from taking hold in the body.
– **Post-Exposure Prophylaxis (PEP)**: If bitten or scratched by an animal suspected of carrying rabies, immediate medical treatment is crucial. PEP consists of:
– **Rabies Vaccination**: A series of rabies shots (usually 4-5 doses) administered over a period of 14 days. These shots boost the body’s immune response to the virus.
– **Rabies Immune Globulin (RIG)**: A concentrated dose of antibodies is administered to neutralize the rabies virus, especially in cases of high-risk exposure (e.g., deep bites, multiple bites, or bites to the face or neck). RIG is injected near the wound site and in other parts of the body to ensure immediate protection.
The success of PEP treatment depends on **how quickly** it is administered after exposure, ideally within **24-48 hours**. If treatment is delayed, the risk of the virus reaching the central nervous system increases dramatically.
#### **Prevention Measures:**
Preventing rabies requires a multi-pronged approach, including vaccination, prompt medical care, and public awareness.
1. **Vaccination:**
– **For Humans**:
– **Pre-Exposure Prophylaxis (PrEP)**: This is recommended for individuals who are at high risk of rabies exposure, such as veterinarians, animal handlers, wildlife workers, and travelers to regions where rabies is prevalent. It involves a series of three doses of the rabies vaccine before exposure.
– **Post-Exposure Prophylaxis (PEP)**: This is given to anyone who may have been exposed to rabies through a bite or scratch from a potential carrier.
– **For Animals**:
– **Pet Vaccination**: Ensuring that dogs, cats, and other domestic animals are vaccinated against rabies is one of the most effective ways to control the spread of rabies in communities.
– **Wildlife Control**: In some areas, wildlife (e.g., raccoons or foxes) are vaccinated through oral rabies vaccines (dispersed in baits).
2. **Animal Control and Monitoring**:
– **Leash Laws**: Keeping pets on a leash or within a controlled environment to avoid exposure to wild animals.
– **Avoiding Contact with Wild Animals**: People should not approach, handle, or try to rescue wild animals. Even apparently healthy animals can be carriers.
– **Vaccinating Strays**: Encouraging vaccination campaigns for stray animals can help prevent rabies in local populations.
3. **Avoiding Risky Areas**:
– Travelers to areas with high rabies risk should avoid direct contact with animals, especially dogs and bats, and seek immediate medical care after any animal bite.
4. **Public Education**:
– **Raising Awareness**: Public education on rabies prevention, including the importance of seeking treatment immediately after an animal bite, is vital to reducing human cases.
– **Informing Pet Owners**: Educating pet owners about the importance of rabies vaccinations for their animals and the dangers of exposure.
5. **Immediate Action After Animal Exposure**:
– **Wound Cleaning**: Clean the bite or scratch site thoroughly with soap and water immediately after exposure to reduce the risk of infection.
– **Seek Medical Attention**: If bitten or scratched by an animal that might have rabies, **seek immediate medical care** to determine whether rabies vaccination is necessary. Rabies treatment is highly effective if administered early.
Also Read About: Animal Injection Administration
—
Rabies remains a **preventable** disease, but once symptoms develop, it is almost always fatal. Prevention through vaccination of both humans and animals, alongside awareness of exposure risks and quick intervention following bites, is essential to controlling and eventually eradicating this deadly disease.